You watch your salt. You take your statin. You walk daily. But what if the biggest driver of your heart risk isn’t in your arteries, but in your digestive tract?
Most heart doctors act like plumbers. They look at your pipes (arteries) and the pump (your heart). If a pipe is clogged, they try to clear it. If pressure is high, they try to lower it. But they often ignore the chemistry factory that controls the whole system: your gut.
This “chemistry factory” is your microbiome. When it isn’t working right, it pumps out toxins that inflame your blood vessels.
In this guide, you will learn about the gut-heart connection. We will look at a hidden compound called TMAO and how it silently damages your heart. Most importantly, you will get a list of cardiovascular risk factors to discuss at your next appointment.
The “TMAO Trap”: How Your Lunch Becomes Plaque

For years, we thought the fat in a steak caused the problem. We were wrong. The real issue is often what your bacteria do with the meat after you eat it.
Here is how it works. When you eat red meat or eggs, you consume nutrients called choline and L-carnitine. Your body needs these. But if you have “bad” gut bacteria, they grab these nutrients and turn them into a gas called TMA.
Your liver then turns that gas into a compound called Trimethlyamine N-oxide (TMAO).
Think of TMAO like super-glue for cholesterol. It stops your body from clearing cholesterol out of your arteries. High TMAO levels also make your blood more likely to clot.
New data from late 2025 connects this to more than just heart attacks. Research now links high TMAO to aortic aneurysms. This is a weakening of the main artery in your body, and it is a serious risk for men over 65. If you eat a lot of red meat, you need to know if you are falling into this trap.
The “Leaky” Inflammatory Engine
The Border Patrol
Your gut lining acts as a strict guard. It lets nutrients in but blocks bacteria.
The Breakdown
Aging & Dysbiosis cause the wall to thin. This is Leaky Gut.
Toxins Escape
Bacterial shells (LPS) slip into the blood. Your immune system attacks, causing inflammation.
Heart Risk
Inflammation stiffens vessels. Plaque bursts. Bloating may be a warning sign for your heart.
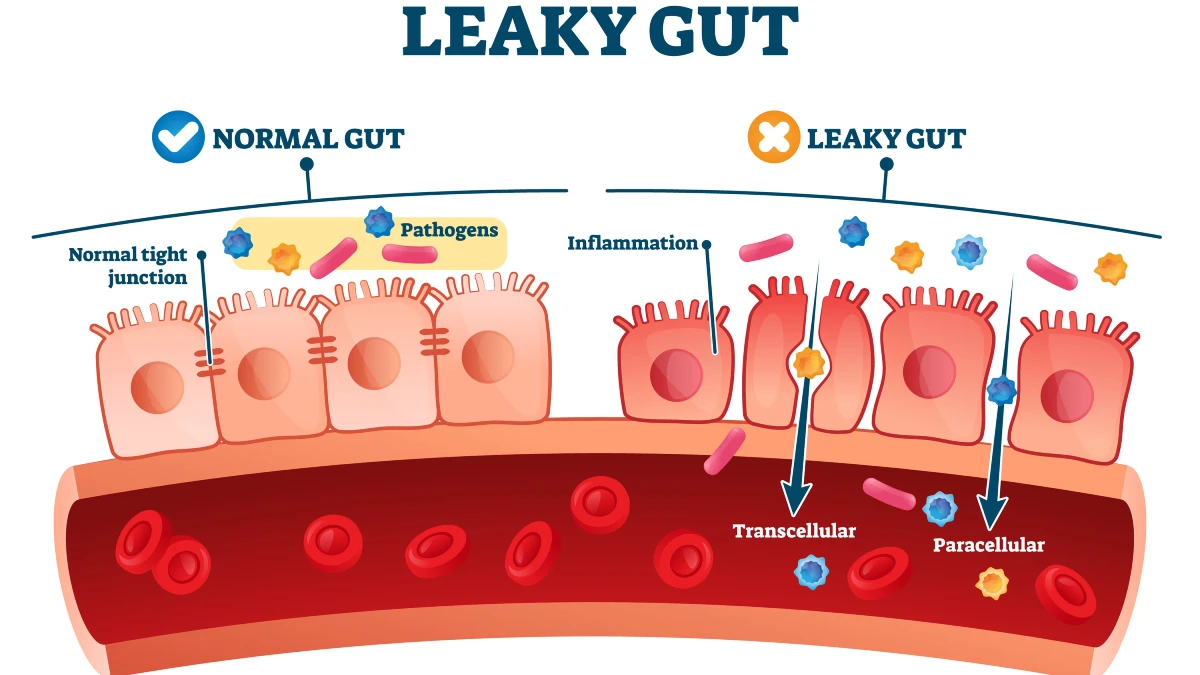
Your gut has a lining that acts like a border patrol. It lets food in but keeps bacteria out.
As we age, this lining gets thinner. If you have an imbalance of gut bacteria (dysbiosis), that lining can break down. Doctors call this “intestinal permeability.” You might know it as “leaky gut.”
When the wall breaks, toxins escape. Specifically, bits of bacterial shells called LPS (lipopolysaccharides) slip into your bloodstream. Your immune system sees these toxins and attacks.
This creates constant, low-grade systemic inflammation.
This inflammation stiffens your blood vessels. It makes plaque in your arteries unstable and likely to burst. This explains why some people have heart attacks even with “normal” cholesterol numbers. Their leaky gut symptoms, like bloating or fatigue, were actually warning signs for their heart.
Statins and Your Gut: A Complicated Relationship

If you are over 50, you or your friends probably take statins. These drugs save lives. But they also change your gut.
Taking statins shifts your microbiome. It tends to increase a type of bacteria called Bacteroides. This isn’t always bad, but it is a change.
The relationship goes both ways. New research suggests your gut bacteria decide if you get statin side effects.
If your gut is healthy and diverse, the drug often works well. If your gut is in bad shape, you might face muscle pain or blood sugar spikes. A healthy gut helps you tolerate the medicine you need.
The “Natural BP Med”: Short-Chain Fatty Acids (SCFAs)

Not all bacteria are bad for your heart. Some are your best allies.
When you eat fiber, good bacteria ferment it. They turn that fiber into “postbiotics.” The most important one is Butyrate.
Butyrate is powerful. It sends chemical signals to your blood vessels telling them to relax. When vessels relax, blood pressure goes down.
This means fiber supplements, like psyllium husk, are more than just bathroom aids. They are natural blood pressure reducers. By feeding your gut fiber, you are helping your body make its own medicine to keep your arteries flexible.
Action Plan: What to Do & Ask Your Doctor

You cannot fix what you do not measure. Here is how to take action on your heart healthy diet plan and medical care.
1. Get the Right Test Don’t guess. Ask your doctor for a TMAO blood test. Major labs like Cleveland HeartLab and Quest now offer this. If your levels are high, you know you have work to do.
2. Swap Your Proteins If your TMAO is high, red meat and eggs are the fuel for the fire. Swap them for plant proteins like lentils, beans, or tofu. These foods do not convert into TMAO. You don’t have to be vegan forever, but a 4-week break can drop your levels fast.
3. Be Careful with Probiotics Don’t just buy the cheapest bottle at the store. Some random strains can increase histamine or inflammation. Look for specific strains like Lactobacillus rhamnosus, which has been linked to better blood pressure control.
Conclusion
Your heart does not work alone. It relies on the chemical signals your gut sends every minute of the day.
If you ignore your digestion, you ignore a huge part of your heart health. Managing your microbiome is the new frontier of cardiology.
So, at your next physical, don’t just check your LDL. Ask your doctor: “Should we test my TMAO levels?” It might be the most important question you ask this year.

